US NEWS: Emergency Services Crews Often Unprepared for Diabetic Crises
Scott Benner
By Serena Gordon
HealthDay Reporter
FRIDAY, Jan. 26, 2018 (HealthDay News) -- If you call 911, you expect to get the medical services you need.
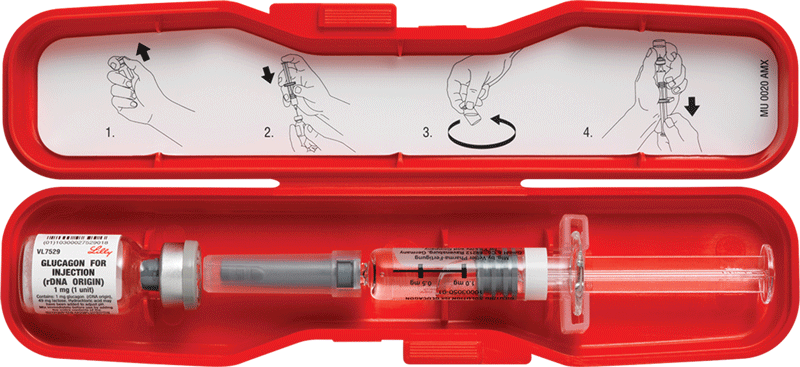
But new research suggests that when it comes to severe low blood sugar episodes in people with diabetes, first responders might not be able to administer a potentially lifesaving medication called glucagon.
Glucagon is an injectable medication that prompts the liver to release stored glucose. This quickly raises blood sugar.
But paramedics can give the injections, said Dr. Craig Manifold, medical director of the National Association of Emergency Medical Technicians. That's because paramedics get between 750 and 1,500 hours of education compared to about 100 to 150 hours of training for EMTs.
Low blood sugar levels (hypoglycemia) generally occur in people with type 1 or type 2 diabetes taking insulin or other blood sugar-lowering medications. Researchers said more than 100,000 serious hypoglycemia episodes occur each year.
Gabbay noted even U.S. Supreme Court justices aren't immune to this problem. Earlier this month, Justice Sonia Sotomayor, who has type 1 diabetes, had to call emergency services for help with serious low blood sugar.
You can read the rest of the article here



















