10 Steps to Take After Your Insurance Denies an Insulin Pump or CGM
Scott Benner
If you haven't already listened to D-Mom and volunteer insurance advocate Samantha Arceneaux on the Juicebox Podcast go ahead and click play on that player you see below. -- Sam is a never ending font of information on how best to appeal your insulin pump or continuous glucose monitor insurance denial and she was kind enough to write this guest post for Arden's Day. The mother to Mikayla a T1 5 year old diagnosed at 22 months old, Samantha has spent the last several years as a volunteer diabetes insurance advocate, helping other parents fight insurance companies for insulin pump and CGM coverage.
Sam is brilliant and these are her 10 steps to take when you've been denied by your evil overlords (medical insurance company).
guest post
Steps When Being Denied by Your Insurance:
- Did you receive a denial letter? If not, investigate to find out why. Was the supplier incorrect? Were they in-network?
- Double check your pharmacy benefits to see if you can gain the item that way.
- If it’s a company plan, ask your HR department if they might be able to override the denial.
- Ask your doctor to complete a peer-to-peer review with the insurance company.
- If still denied, ask the doctor for a letter of medical necessity.
- Look at why they are denying, then compare against your medical records and the insurance’s medical/clinical policy or guideline. Find if they incorrectly applied their policy to your situation, or if they are using outdated data.
- Do your research. See if there are new studies that prove your medical request is supported by professional recommendations or research studies. Aim to have 2-5 relevant studies/statements.
- Go for the appeal. Insurances want a medical need established and why it (the item being requested) has the potential to lower their costs. It cannot be emphasized enough, what you put into it is what you can expect to get out of it.
a) Include what the system/supply does medically in a few short sentences, don’t assume they know. It will make the rest of your arguments more effective if they understand the concept behind the device/supply.
b) A modicum of formality can be helpful as well, as the insurance will be unsure of who actually wrote it; was this the patient, an advocate, an attorney, a doctor? It may imply to the insurance reviewer that you are not going away easily.
c) Fight against any outdated research the insurance uses in their medical policy, or if they failed to gather/review your medical data that supports your need for the device/supply.
d) Quotes from the research studies or statements are helpful, since they will not be looking up the studies themselves. Paraphrasing is also encouraged. Just remember to cite the study/professional organization each time.
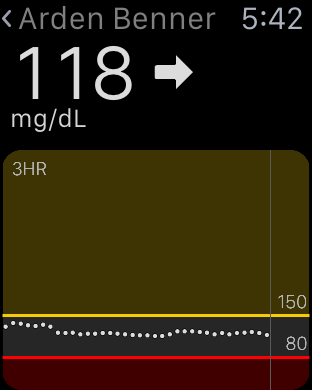
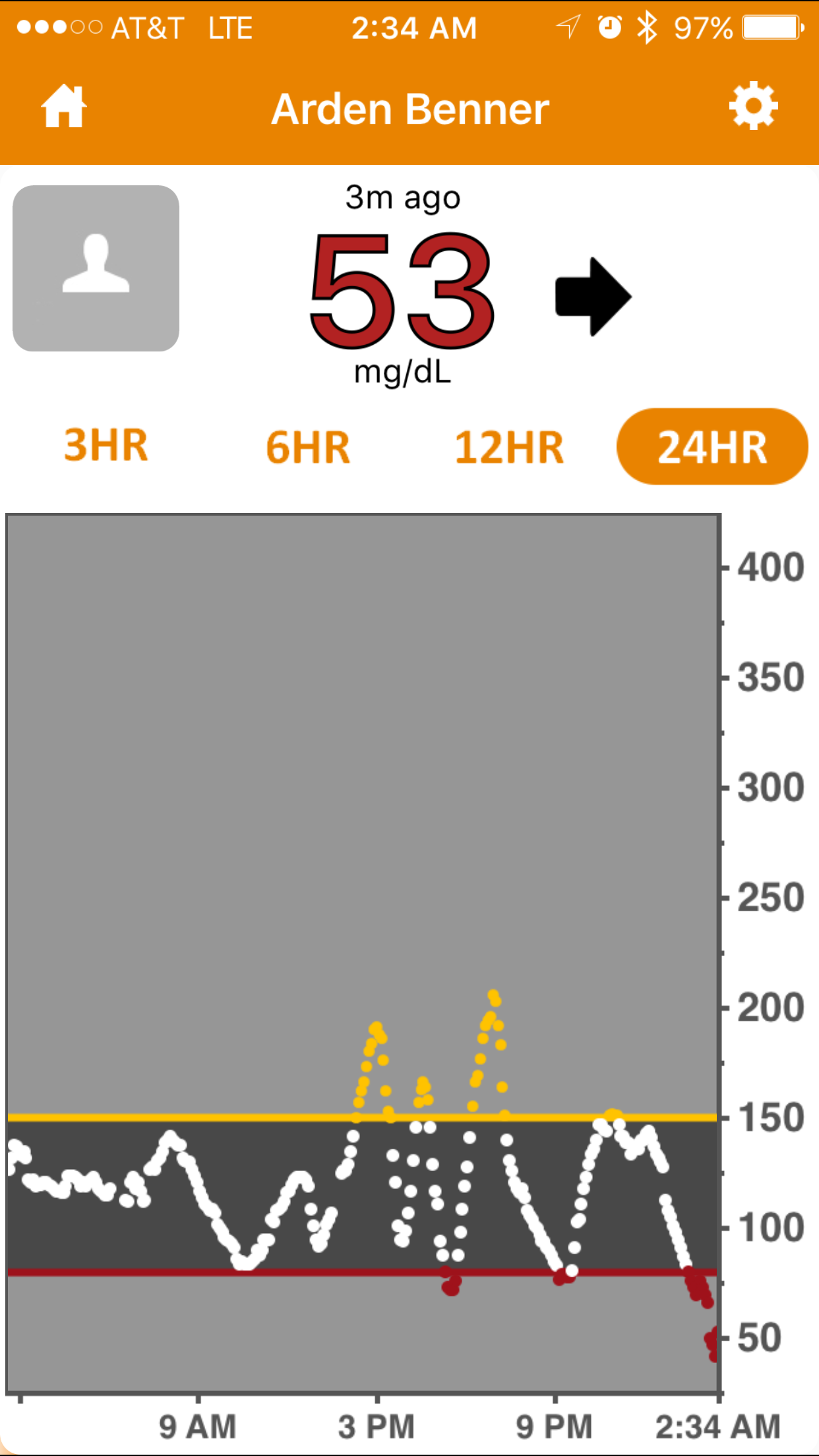
e) Give real life examples on how this device/product can help you (refrain from convenience examples). For instance, do not talk about how a CGM can be remotely viewed and how this saves the hassle of checking in with your child. Rather, talk about how the device alerts you to rapidly changing glucose values so that you can take steps to prevent a crisis from - So you win the appeal and get approval. I strongly advise getting it in writing before you order the supply/device. This will be your evidence in the event something isn’t properly posted in their system, such as length of approval (should be for 1 year).
- If you do not overturn the denial on appeal, try again. Typically you will have two internal reviews that are done by the insurance companies before going on to the external review. The external review is completed by independent reviewers and tends to be more impartial, which means a higher chance of getting approved. (Medicaid/Medicare products may have more levels of appeal available).
Other useful information:
For non-covered items: You will need to request a formulary exception. This means that you recognize that it isn’t a covered product but still feel that it is medically necessary and should be covered by your insurance. Treat this as an appeal situation.
For non-preferred items: If a drug or supply is non-preferred, you will ask for a tier exception. This is basically where you give the insurance company a medical reason why you cannot utilize the preferred item and ask that they give you the non-preferred item AT the preferred rate. This typically is a pharmacy situation.
Visit Sam's blog to read her other detailed information regarding insurance denials. Sam rocks!